
In contrast, other studies report that combination therapy is not cost-effective 20, 28 compared to statin therapy. The availability of Ezetimibe as a generic drug in several countries 25 can act as a positive indicator and increase overall access to this medication.įurther, the evidence on the cost-effectiveness of this therapy is also inconsistent, as few studies report it is cost-effective 26, 27.
However, its use and the extent to which it meets unmet reuirements are limited. As a result, Ezetimibe can be used as a next-cholesterol medication. Furthermore, a recent meta-analysis of cost-utility studies (CUA) showed PCSK9i to be not cost-effective compared to other lipid-lowering therapeutic agents in high-income countries (HICs) 23, 24. A favourable tolerability profile, ease of use, and affordability make Ezetimibe a better option than PCSK9i 22.
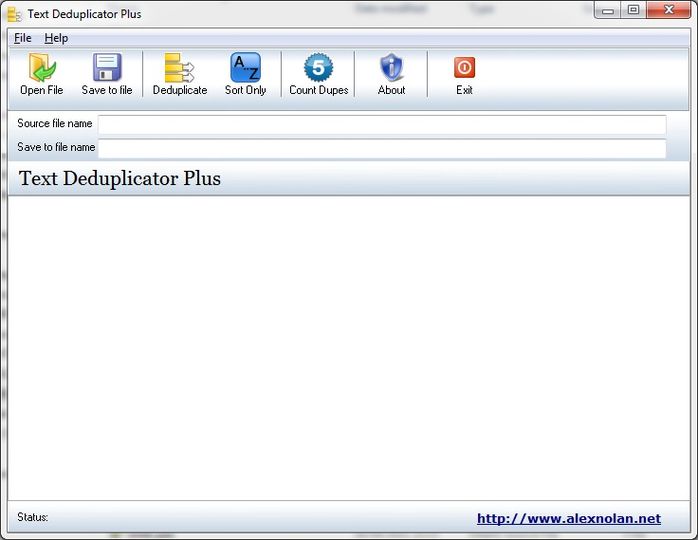
TEXT DEDUPLICATOR PLUS PROFESSIONAL
Many professional organisations have recently issued guidelines recommending the use of non-statin medications in clinical practice, consideringtheir usefulness 3, 18- 20.Įzetimibe co-administration with statins has resulted in fewer very-high-risk and extremely high-risk patients eligible for other lipid-lowering agents 21. Studies showed that Ezetimibe reduced LDL-C at levels consistent with Cholesterol Treatment Trialists’ (CTT) Collaboration estimates, giving CTTs’ extrapolation beyond their intial analysis legitimacy and validity 15, 17. Hence, the 2018 Cholesterol guidelines warrant using Ezetimibe in individulas with a high ASCVD risk despite receiving optimal statin medication 7. When added to a statin, Ezetimibe achieves a reduction in LDL-C of typically 20–25% with reduced atherosclerotic CVD (ASCVD) risk 15, 16. It is used to achieve the desirable LDL-C levels for patients on maximally tolerated statin therapy. Ezetimibe is a non-statin lipid-modifying agent targeting the Niemann-Pick C1-like 1 intestinal cholesterol transporter protein (cholesterol absorption inhibitor) 13, 14. Despite rigorous statin regimens aimed to lower the risk of cardiovascular complications, a large number of statin-treated patients fail to attain the recommended target low-density lipoprotein-cholesterol (LDL-C) levels due to statin intolerance or discontinuation of treatment due to adverse drug reactions 11, 12. Statins lower the cardiovascular risk in all groups 6- 8, as well as the risk of developing CVD events 9, 10.
For reducing cardiovascular events, statin drugs targeting 3-hydroxy-3-methyl-glutaryl-coenzyme (HMG-CoA) reductase are the most prescribed medications 5. The World Health Organization (WHO) reported that an estimated 17.9 million people died from CVDs in 2019 alone, representing one-third of all global deaths 4. Cardiovascular disease (CVD) and cardiovascular events have a perpetual relationship with hyperlipidemia 1- 3.


 0 kommentar(er)
0 kommentar(er)
